Elite Hair Centers
We know that choosing a hair restoration provider is an important decision. At Elite Hair Centers, our unique dermatology and plastic surgery team is dedicated to delivering exceptional results with expertise and passion. This is what sets us apart from the competition.
Hair Loss Evaluation
Hair loss can be emotional and distressing, and determining the underlying cause is important for effective treatment. A detailed history can help to evaluate and properly diagnose the condition. Understanding the pattern, duration, and extent of hair loss can reveal important information about the underlying cause. Additionally, we want to know about any associated symptoms, as well as, family history. Hair loss that occurs on the top of the scalp in an adolescent male with a strong family history of similar hair loss, for example, may be hereditary, whereas focal patches of scaling or smooth hair loss may indicate a completely different disease process.
We will want to differentiate between hair shedding, hair thinning, and hair breakage. Active hair shedding is characteristic of alopecia areata and telogen effluvium, whereas androgenetic alopecia is characterized by progressive hair thinning (although some patients will report shedding as well). A telogen effluvium can be induced by a number of possible factors – new medications, calorie/protein restriction, significant weight loss, illness, surgery, iron deficiency, pregnancy, and even emotional stress – so it is good to know if any of those are relevant. Likewise, women with pattern hair loss may report irregular menstrual cycles or infertility.
Hair breakage may indicate hair care practices that damage the hair shaft or possibly hereditary conditions. This may include chemical treatments, high heat, or prolonged traction on the hair shafts. Fungal infections on the scalp can also cause abnormal hair breakage, typically in the setting of itching and scaling. Finally, trichotillomania (or twisting/pulling out hairs) can present with broken hair shafts.
In conclusion, obtaining a thorough history of the patient’s hair loss can provide valuable insight into the underlying cause. We can make an accurate diagnosis and provide the most effective treatment if we understand the pattern, duration, and type of hair loss.


CLINICAL EXAMINATION
A physical exam of the hair and scalp is an important next step, with particular attention paid to the presence or absence of follicular openings. If follicular units are seen in the affected area, then we are likely dealing with a non-scarring alopecia. If no follicular ostia/units are seen in the area of hair loss, this would suggest a scarring alopecia and is associated with a certain set of conditions.
The pattern and distribution of hair loss will be assessed, including an estimate of the hair density. For pattern hair loss, it may be helpful to examine the density of the front and top of the scalp to the posterior scalp. And in women, it may be helpful to examine the width the midline part. The scalp will be inspected for erythema, scales, papules, pustules, erosions, or excoriations which can be clues to a diagnosis. Finally, the caliber, fragility, length, and shape of the hair shaft can also be evaluated.

Trichoscopy
A dermatoscope can be used to further examine the hair and scalp (trichoscopy) at higher magnification. This allows one to search for additional clues by examining the follicular openings/ostia, hair shafts for morphology and size (including variation in size to determine the number of hairs which are vellus vs terminal), and pattern of scale.

PULL TEST
A pull test can provide valuable information, in which 50-60 hairs are gently pulled from the scalp. If more than 6 (10%) of the hairs are released during the test, this may indicate a positive test, and is an indication of active hair loss. It is critical to note that the individual should refrain from washing their hair for at least 24 hours prior to the pull test, as this may lead to a false negative. The hairs that are extracted can then be examined – either with one’s eyes, a dermatoscope, or potentially a microscope. Typically, the hairs that come out will be telogen hairs, which could indicate a telogen effluvium or alopecia areata. However, abnormal anagen hairs can be pulled out, as seen in cases such as anagen effluvium or loose anagen syndrome.
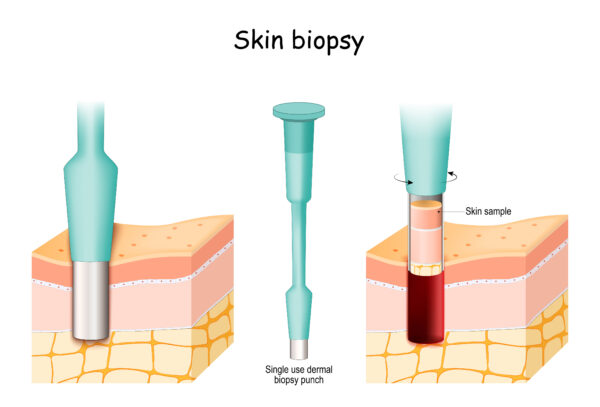
Scalp Biopsy
A scalp biopsy is typically highly informative and may be recommended if the diagnosis is not clear with the prior methods. In this case, a 4 mm punch tool is used to extract a core of tissue from the area of active hair loss. This piece of tissue is taken to the lab where it is processed and interpreted by a dermatopathologist (like Dr. Fischer). There is variability from lab to lab and it is also dependent on the pathologist, but typically the biopsy is cut horizontally at various levels throughout the specimen. This allows each hair follicle to be examined at different levels including the infundibulum, isthmus, and bulb. The pathologist is able to assess the total number of follicles, calculate the terminal/vellus hair ratio, calculate the number of hairs in telogen phase, detect the presence and distribution of inflammation, as well as, the presence of early or advanced scarring.

LABS
Laboratory tests can sometimes be helpful in determining the underlying cause of hair loss. Serum ferritin levels, for example, may be checked to assess for iron deficiency anemia as a cause of hair loss, particularly in women who have ongoing shedding. Thyroid function tests, including thyroid-stimulating hormone (TSH), may be required as part of a comprehensive workup. Free testosterone and dehydroepiandrosterone sulfate (DHEAS) levels should be measured in women who exhibit signs of virilization, such as irregular menstrual cycles, hirsutism, infertility, or persistent acne. If lupus is suspected, a serum antinuclear antibody (ANA) test is indicated.
TESTIMONIALS

Before & After Gallery
*Individual results may vary.

